Abstract
Background Significant disparities in AML have been reported in the non-Hispanic black (NHB) population compared to Caucasians. Much less is known about the disparities seen in Hispanics (H), who face unique barriers to healthcare access and treatment. Recent reports suggest that Hispanics have decreased overall survival (OS) compared to non-Hispanic whites (NHW) despite higher prevalence of favorable cytogenetics, younger age at diagnosis and similar rates of chemotherapy. We conducted a single center study investigating the outcomes of AML patients treated at a non-transplant safety net hospital in Texas where the majority of the population is Hispanic. Our primary goal was to compare the impact of race/ethnicity on outcomes and further evaluate the underlying genomic differences between these groups.
Methods We reviewed the medical records of 162 adult AML patients treated at Parkland Health (Dallas, TX) from January 2007 to June 2022. Demographics, baseline disease characteristics including cytogenetics and genomic profile, and AML directed therapies were collected. Patients were grouped based on race/ethnicity into H, NHW and NHB populations. Cytogenetic risk was classified as favorable, normal, complex or other, per the 2017 European Leukemia Net (ELN) risk classification. Genomic testing was performed using the FoundationOne Heme panel. Overall AML risk was classified per 2017 ELN stratification. Response was assessed using the IWG criteria. Categorical and continuous variables were compared using Chi square test and Kruskal-Wallis one-way analysis of variance. OS plots were calculated using Kaplan Meier method, and groups were compared using log rank testing. Multivariable Cox proportional hazard model was used for survival analysis.
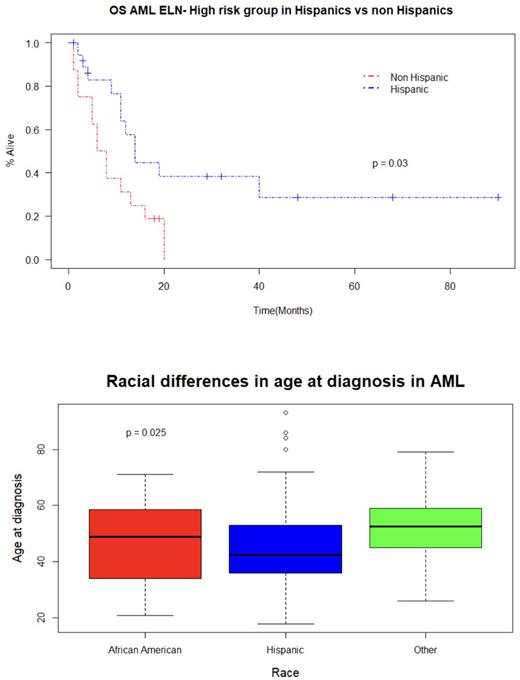
Results In our cohort of 162 patients, 82 (50.6%) were Hispanic (H), 36 (22.2%) were NHB and 44 (27.2%) were NHW. Hispanics were diagnosed at a significantly younger age compared to NHB (42.5 years (y) vs 49 y) and NHW (42.5 y vs 52.5 y, p=.02). Hispanics were found to have higher rates of complex cytogenetics (20.3% for H vs 11.8% for NHB vs 9.5% for NHW), similar rates of favorable cytogenetics (20.3% vs 20.6% vs 19.0%) and lower rates of normal cytogenetics (29.1% vs 44.1% vs 40.5%). Hispanic patients had a lower frequency of NPM1 mutations (p=.058) and higher frequency of CEBPA, NRAS, MLL, WT1, RUNX1 and TET2 mutations. Per ELN risk classification, Hispanics were less likely to have favorable risk AML (23.2% vs 36.1% vs 29.5%) and more likely to have intermediate (53.7% vs 44.4% vs 50.0%) or high-risk disease (23.2% vs 19.4% vs 20.5%) than NHB and NHW. Hispanics were less likely to receive intensive induction chemotherapy with 7+3 (85.4% vs 97.2% vs 90.9%), despite their overall younger age of presentation, but achieved similar remission rates post frontline therapy (78.0% vs 86.1% vs 75.0%). Hispanics had a numerically longer OS compared to NHB and NHW (mOS 43 months (m) vs 17 m, vs 14 m), although differences were not statistically significant (p=.20) likely due to the small size of the cohort. When Hispanics were compared against a combined cohort of NHB/NHW, they had longer OS in the high-risk group (p=.03). In a multivariate Cox regression analysis, OS was negatively associated with age at diagnosis (HR 1.022, p=.0063) and intermediate or high ELN risk (HR 3.431, p=.0002 and HR 4.689, p=3.84 x 10-05 respectively) and positively associated with Hispanics (HR .614, p=.0259). In our cohort, only 14 patients (8.6%), 3 of which had high risk disease, were able to proceed to transplant.
Conclusion Our study of underserved patients with AML demonstrate a younger age at presentation for Hispanics but suggest that, contradictory to previously reported results, Hispanics have improved overall survival, particularly in the high-risk group, compared to NHB/NHW in the non-transplant setting. Our results may suggest that when healthcare access is not a barrier to treatment, Hispanic patients with AML can have similar, if not improved, outcomes to other populations. However, access to transplant remains a major barrier that needs to be further addressed to improve outcomes for this patient population.
Disclosures
Madanat:Sierra Oncology, Stemline Therapeutics and Novartis: Membership on an entity's Board of Directors or advisory committees; BluePrint Medicines, GERON, OncLiv: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal